1. Introduction- Veterinary Radiology
The production of a radiograph involves the use of complicated apparatus and a sequence of complex physical processes. A basic understanding of radiological physics will allow the radiographer to make the best use of the equipment available.
RadioGraphy – the processes involved in getting a radiograph
RadioLogy – the procedure of looking at a radiograph
2. The Electromagnetic spectrum and ionising radiation
- X-Rays form only one part of the electromagnetic spectrum, which includes radio waves, microwaves (radar, heating etc.), infra-red, visible light, ultraviolet light, X-Rays and gamma rays.
- These radiations all have a few common properties:
- They do not require a medium for propagation
- They are transmitted by combined electric and magnetic fields
- They travel with the same velocity in a vacuum
- They travel in straight lines
- They may interact with matter and be absorbed or scattered
- They have the characteristics of both transverse waves and discrete particles photons)
- The energy of a photon is equal to the frequency multiplied by Planck’s constant
- Thus photons of short wavelength have high frequency and high energy
- These photons are useful in diagnostic radiology
3. Properties of X-Rays
- Fluorescence
- X-Rays cause certain substances to fluoresce, i.e. to emit light in the visible spectrum after absorbing X-rays
- Such substances include calcium tungstate or rare-earth phosphors, both found in intensifying screens (q.v.)
- Photographic effect
- X-Rays produce a ‘latent image’ (invisible to the eye) on photographic film
- This image is made visible by processing the film
- Penetration
- X-Rays can penetrate substances or tissues that are opaque to visible light
- They are gradually absorbed the further they pass through an object
- The amount of absorption depends on the atomic number and density of the object and on the energy of the X-Rays
- Excitation and ionisation
- X-Rays produce excitation and ionisation of the atoms and molecules of the substances through which they pass
- Excitation is the process of raising an electron to a higher energy level
- Ionisation is the process in which an electron is completely removed from an atom
- Biological effect
- X-Rays interact with living tissue and can cause biological changes
- These changes are mediated directly by excitation or ionisation of atoms or indirectly as a result of chemical changes occurring near the cells
- Affected cells may be damaged or killed
- Genetic effects involve chromosomal damage or mutation in the reproductive cells and will affect future generations
- Somatic effects involve damage to the other tissues and result in changes within the individual’s lifetime (e.g. radiation burns, leukemia)
- Radiation is a particular hazard because its effects are painless, latent and cumulative
- SO QUIT COMPLAINING AND WEAR THE PROTECTIVE EQUIPMENT AND YOUR BADGE!!!
4. The X-Ray tube
1. Since electrons are produced when fast-moving electrons are slowed down or stopped, there are three basic requirements for X-Ray production in an X-Ray tube:
- A source of electrons (cathode)
- A target to stop the electrons (anode)
- A method of accelerating the electrons from the source to the target (high potential difference between the two)
- The cathode:
- Electrons are produced by heating a filament by thermionic emission
- The number of electrons which pass from the cathode to the anode represents the tube current and is measured in milliamperes (mA)
- The tube current can be controlled by the radiographer
- The anode
- The anode is maintained at a high positive potential with respect to the cathode during the exposure
- Electrons emitted by the filament are therefore accelerated to the anode and strike the target
- The potential difference between the cathode and the anode is measured in kilovolts (kV), and can be controlled by the radiographer
- X-Rays are produced at the anode when it is struck by electrons; but only 1% of the incident energy is converted to X-Rays. The remainder is converted into heat, and must be dissipated
- A fixed anode relies on conduction of the heat away from the target by mounting it on a copper stem
- A rotating anode allows X-Rays to be produced over a greater area of the target by rotating it during the exposure
5. Factors affecting the quality and intensity of beam
- Quality is a measurement of the penetrating power of the X-Ray photons. The quality of the beam increases as the proportion of high energy photons increases
- Intensity is a measure of the amount of radiation produced
- Various factors affect the quality and intensity of the beam
- kV – the greater the potential difference across the tube, the faster the electrons move and the higher the energy of the X-Ray photons. Thus the quality and intensity are increased
- mA – the higher the tube current, the greater the intensities of all the photon energies, and the intensity of the beam is increased
- time – the longer the exposure, the greater the time during which X-Rays are produced, and the greater the beam intensity. The time (seconds) and mA are generally considered together as the composite factor mAs. mA x time = mAs
- distance – increasing distance from the source of radiation results in a decrease in the intensity of the beam, according to the inverse square law. Hence doubling the distance from the tube head will result in a beam of one quarter its original intensity
6. Interaction of X-Rays with matter
- When a beam of X-Rays passes through matter, its intensity is reduced as the energy is absorbed or scattered
- The degree of attenuation depends on the atomic number and physical density of the tissue, and the energy of the X-Rays
- The differential absorption of X-Rays by the various tissues of the patient allows a radiographic image to be made
- 1. Air
- 2. Fat
- 3. SoftTissue
- 4. Bone
- 5. Metal
7. Properties of radiographic film and formation of the image
- X-Rays will produce a pattern of varying depths of blackness on the film
- The incident photons are attenuated to varying degrees by the patient’s tissues
- The emerging pattern of photons of differing energies affect the film emulsion to produce the latent image
- Developing the film allows this image to become visible
- The film emulsion consists of gelatin containing finely dispersed grains of silver bromide
- The absorption of X-Rays by the silver bromide grains renders them developable
- Silver bromide grains which have been exposed to X-Rays will be turned black by the developer
- Unexposed grains are dissolved and removed and leave a white area on the film
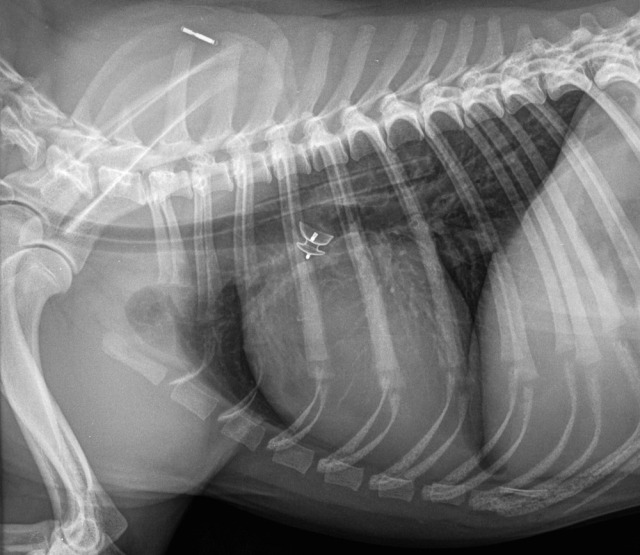
Consider the possibilities when making a radiograph of a patient’s thorax:
- Some rays do not penetrate the chest at all, and are only slightly attenuated by air.. Therefore the maximum number of photons will pass through to the film. This causes maximum exposure of that part of the film, causing blackening of the film
- Some rays pass through the body wall and the lung. The body wall will absorb a number of photons, but few photons are absorbed by the aerated lung.
Therefore the film will receive a medium exposure - Some rays pass through the body wall, mediastinum and heart.
Most of the photons will be absorbed, and only a few pass on to the film.
This results in a low exposure of that part of the film, causing a relatively white area to be seen on the film
8. Effect of the exposure factors on the film
- kV: governs the penetrating power of the photons
- Films taken with a low kV have high contrast, i.e. tissues appear black or white with very little grey
- Films taken with a high kV have low contrast, i.e. the film is more uniformly grey (a flat film)
- mAs: governs the amount of X-Rays reaching the film
- mAs too low (underexposure) results in a pale film
- mAs too high (overexposure) results in a dark film
- Distance: affects the amount of X-Rays reaching the film by the inverse square law
- This will only affect the film if the distance is changed without altering the mAs
- In essence, the kV controls the number of shades of grey, and the mAs controls how dark they are
9. Cassettes and intensifying screens
1. A cassette is a light-tight, robust container which will:
- Hold the film and intensifying screens in close contact
- Protect the film from visible light, since this will blacken the film as well as X-Rays
- Protect the film and screen from damage during use
- Two intensifying screens are present within the cassette, either side of the film
- Screens contain materials which fluoresce when bombarded by X-Rays
- The radiographic film is sensitive to this visible light emitted by the screens as well as the X-Rays themselves
- The use of both ]visible light and X-Ray photons allows the reduction of exposure times
- However, film without screens or a cassette is used when very fine detail is required (Paper cassettes- require very long exposure times, usually a full second)
10. Qualities of a good diagnostic radiograph
- An accurate portrayal of the structures under examination, which requires good positioning with the minimum of geometric distortion (the region of interest should be under the central ray, parallel to and close to the cassette)
- Easy perception of the relevant structures with good contrast and detail
- No misleading artifacts
11. Objective qualities of a good radiograph
- Contrast
- This is the difference in blackness between two adjacent tones
- Films with high contrast will show a white bone on a uniformly black background
- Films with a low contrast will show no black or white, but only tones of grey
Contrast is affected by
- kV: low kV gives high contrast
- mAs: low mAs gives low contrast
- inherent properties of the radiographic film
- processing: development affects contrast
- scattered radiation produced within the patient reduces contrast
- fog:
- inherent in the film
- exposure to visible light or incorrect safe light in dark room
- overdevelopment
- Detail and definition
- The details of a radiograph depend for their perceptibility upon their contrast with the background and upon their definition or sharpness
- Contrast has been dealt with above, however, it is important to note:
- Very small details require high contrast if they are to be easily seen
- If one opacity merges gradually into another, the eye will find it difficult to perceive the difference
- If two densities are separated by a firm line of demarcation, the difference can easily be seen
- Definition is poor if there is a blurred image, which may be caused by:
- factors inherent in the tube head and film/screen combination
- movement of the machine, animal or film during exposure
12. Identification of radiographs
- All films must be adequately labeled and show
- The name of the hospital or practice
- The date
- The patient identity or case number
- Various methods are available
- Lead letters
- Lead-impregnated tape
- Film camera: exposes the information into the emulsion
- Additional information may need to be incorporated
- Left/right marker to identify limbs or radiographic projection
- Indication of time elapsed in a sequential study
- Pre- and post-operative pictures
Radiographs are part of the medical record and MUST BE ADEQUATELY AND ACCURATELY LABELED.
13. Radiation safety
ALARA is a philosophy of excellence used in one’s day-to-day work with radioactive materials and radiation sources. It is when one strives to keep one’s radiation exposure As Low As Reasonably Achievable.
Persons operating X-ray equipment should practice dose reduction methods whenever using the equipment.Basic safety measures include keeping exposure time short, keeping distance from the source large, and using appropriate shielding, such as lead aprons. All users of X-ray equipment must have specific training as provided by their supervisor.
Human fingers (or any other parts) should NEVER!!! be present in the radiograph.
Lead gloves do not provide protection from the primary X-ray beam. In other words, wearing a lead glove and putting your hand in the radiograph offers no protection at all. The lead only protects the hands from scatter radiation arising at the periphery of the radiographic image.
- Protection of the radiographer
- Personnel should never be in the primary beam
- Patients should not be held during an exposure unless it is clinically necessary, i.e. sedation or general anesthesia is required in many cases
- All persons participating in the examination should wear appropriate protective clothing (lead rubber aprons, gloves/sleeves)
- Persons not involved in the radiographic examination should be excluded from the room
- The room should be large and have protective screens for use during exposure
- Appropriate dosimeters should be worn to identify if unacceptable exposure to X-Rays is occurring
- Protection of the patient
- Use the fastest film/screen combination possible to obtain diagnostic pictures
- Collimate the primary beam to include only the area of interest
- Use a reasonable film-focal distance
- Avoid repeat radiographs by ensuring proper exposure and development
- Protection of the public
- Doors and walls should be treated as required to prevent escape of radiation
- Warning lights should be placed outside the radiography room to signal tube preparation and exposure
- Radiation warning signs should be present on the doors
- People under the age of 18 and pregnant women should not be allowed to assist in radiographic procedures
The majority of the text is from: http://www.priory.com/vet/physint.htm